A common over-the-counter (OTC) medication, diphenhydramine, widely used in sleep aids like Benadryl, Unisom SleepGels, and ZzzQuil, has been linked to an increased risk of dementia with long-term use, prompting concerns among healthcare professionals and consumers.
Long-term use of diphenhydramine, a first-generation antihistamine, might elevate the risk of dementia, sparking warnings from medical experts about its potential cognitive impacts. The medication is commonly found in numerous over-the-counter (OTC) sleep aids and allergy medications, making it easily accessible to a broad population. Concerns have been raised regarding the cumulative effect of diphenhydramine on brain health with prolonged usage, leading to recommendations for cautious and informed consumption. This has prompted calls for further research to fully understand the scope and mechanisms of these risks, as well as increased awareness among consumers and healthcare providers about safer alternatives for managing sleep issues and allergies. The link between diphenhydramine and dementia underscores the need for vigilant monitoring and evaluation of OTC medications’ long-term effects, advocating for a balanced approach between immediate relief and long-term cognitive well-being.
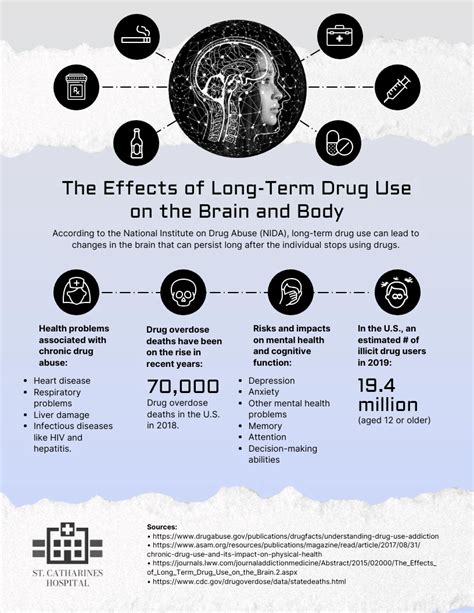
Diphenhydramine, a first-generation antihistamine, works by blocking histamine receptors in the brain, which can cause drowsiness. While effective for short-term relief of allergies and insomnia, its long-term use has been associated with several anticholinergic effects that can negatively impact cognitive function. Anticholinergic effects occur because the drug blocks acetylcholine, a neurotransmitter vital for memory and learning. Studies have indicated that prolonged exposure to anticholinergic drugs like diphenhydramine can lead to cognitive decline, memory impairment, and an increased risk of dementia. The cumulative effect of these anticholinergic properties raises concerns about the safety of using diphenhydramine-containing medications regularly over extended periods. Health experts emphasize that while occasional use is generally considered safe, chronic use should be approached with caution, especially in older adults who are more susceptible to the drug’s adverse cognitive effects. This highlights the importance of exploring alternative treatments and consulting healthcare providers before committing to long-term use of diphenhydramine-based products.
Medical professionals are increasingly advising patients to explore alternative treatments for sleep and allergy issues due to the potential long-term cognitive risks associated with diphenhydramine. The growing body of research linking prolonged use of diphenhydramine to an increased risk of dementia has spurred recommendations for safer alternatives. These alternatives include non-drug therapies such as cognitive behavioral therapy for insomnia (CBT-I), which helps address the underlying causes of sleep problems without relying on medication. For allergy relief, options like second-generation antihistamines (e.g., cetirizine, loratadine, fexofenadine) are preferred due to their lower anticholinergic effects and reduced risk of cognitive impairment. Lifestyle adjustments, such as maintaining a regular sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques, are also encouraged as part of a holistic approach to managing sleep and allergy symptoms. Consulting with healthcare providers to evaluate individual needs and explore personalized treatment plans is emphasized to minimize reliance on potentially harmful medications like diphenhydramine. This shift towards safer alternatives underscores a broader effort to promote long-term cognitive health while effectively managing common conditions.
The concerns surrounding diphenhydramine use are particularly relevant for older adults, who are more vulnerable to the drug’s anticholinergic effects. As individuals age, their bodies become less efficient at clearing drugs, leading to higher concentrations of diphenhydramine in the system and prolonged exposure to its adverse effects. Older adults also tend to have a reduced supply of acetylcholine, making them more susceptible to the cognitive impairments associated with anticholinergic drugs. Studies have consistently shown that the use of anticholinergic medications in older adults is linked to a higher risk of cognitive decline, memory problems, and dementia. Given these increased risks, healthcare providers often recommend that older adults avoid or minimize the use of diphenhydramine-containing medications and seek safer alternatives for managing sleep and allergy symptoms. Educating older adults about the potential risks and promoting non-pharmacological interventions are crucial steps in safeguarding their cognitive health. This targeted approach recognizes the unique vulnerabilities of older adults and aims to reduce the burden of cognitive impairment associated with diphenhydramine use.
“The issue is the cumulative effect,” says Dr. Michael Munger, president-elect of the American Academy of Family Physicians. He highlighted that occasional use is unlikely to cause harm, but regular, long-term use could pose significant risks. Dr. Munger’s warning underscores the importance of understanding the potential long-term consequences of frequently using diphenhydramine-containing medications. While these drugs are effective for short-term relief of allergies and insomnia, the cumulative effect of their anticholinergic properties can lead to cognitive decline and an increased risk of dementia over time. This concern is particularly relevant for individuals who rely on these medications regularly to manage chronic conditions or sleep disturbances. Dr. Munger’s emphasis on the cumulative effect serves as a critical reminder for both patients and healthcare providers to carefully evaluate the risks and benefits of long-term diphenhydramine use and to explore safer alternatives whenever possible. This proactive approach aims to minimize potential harm and promote long-term cognitive well-being.
Experts recommend that individuals explore alternative treatments and consult healthcare professionals to address underlying sleep or allergy issues rather than relying on diphenhydramine as a long-term solution. This approach emphasizes the importance of identifying and treating the root causes of sleep disturbances and allergic reactions, rather than simply masking the symptoms with medication. For sleep problems, cognitive behavioral therapy for insomnia (CBT-I) is often recommended as a first-line treatment. CBT-I addresses the underlying psychological and behavioral factors that contribute to insomnia, such as negative thoughts about sleep and unhealthy sleep habits. For allergy management, second-generation antihistamines like cetirizine, loratadine, and fexofenadine are preferred due to their lower anticholinergic effects and reduced risk of cognitive impairment. Consulting with healthcare professionals allows for a comprehensive evaluation of individual needs and the development of personalized treatment plans that minimize reliance on potentially harmful medications like diphenhydramine. This proactive and holistic approach aims to promote long-term health and well-being by addressing the underlying causes of common conditions and reducing the risk of adverse effects associated with long-term medication use.
The FDA requires warnings on diphenhydramine-containing products about potential drowsiness, but there is no specific mention of long-term cognitive risks. This discrepancy highlights a critical gap in consumer information regarding the potential long-term effects of diphenhydramine use. While the immediate side effects of drowsiness and impaired cognitive function are acknowledged on product labels, the cumulative risk of cognitive decline and dementia associated with prolonged exposure is not explicitly addressed. This lack of clear warning about long-term cognitive risks may lead consumers to underestimate the potential harm of regular diphenhydramine use, especially when self-medicating for sleep or allergy symptoms. The absence of specific warnings underscores the need for enhanced regulatory oversight and improved communication to ensure that consumers are fully informed about the potential risks and benefits of all medications, including over-the-counter drugs like diphenhydramine. This would empower individuals to make more informed decisions about their health and to take appropriate precautions to protect their long-term cognitive well-being.
The study that fueled the concerns about the long-term effects of diphenhydramine was published in JAMA Internal Medicine in 2015, and it found a significant association between cumulative anticholinergic use and an increased risk of dementia. The 2015 study, led by researchers at the University of Washington, analyzed data from a large cohort of older adults and found that those who used anticholinergic drugs, including diphenhydramine, for an extended period had a higher risk of developing dementia compared to those who did not use these medications. The study specifically looked at the cumulative dose of anticholinergic drugs, meaning that the risk of dementia increased with the total amount of the medication used over time. This finding underscored the importance of considering the long-term cognitive effects of medications, particularly those with anticholinergic properties. The JAMA Internal Medicine study served as a pivotal piece of evidence that prompted increased awareness and concern about the potential cognitive risks associated with diphenhydramine and other anticholinergic drugs. This landmark research has significantly influenced clinical practice and public health recommendations regarding the use of these medications, especially in older adults.
Consumers are urged to review their medication lists, including over-the-counter drugs, and consult with healthcare providers about any concerns regarding diphenhydramine or other anticholinergic medications. This proactive step is crucial for individuals who regularly use diphenhydramine-containing products to manage sleep or allergy symptoms. By reviewing their medication lists, consumers can gain a better understanding of their overall exposure to anticholinergic drugs and assess their potential risk of cognitive impairment. Consulting with healthcare providers allows for a thorough evaluation of individual needs, medical history, and potential drug interactions. Healthcare professionals can provide personalized recommendations on safer alternatives, lifestyle modifications, and strategies to minimize reliance on diphenhydramine. This collaborative approach empowers consumers to make informed decisions about their health and to take appropriate measures to protect their long-term cognitive well-being. It also underscores the importance of open communication between patients and healthcare providers to ensure that medication regimens are safe, effective, and aligned with individual health goals.
While short-term use of diphenhydramine is generally considered safe for occasional allergy or sleep relief, the risks associated with long-term use necessitate a careful evaluation of alternative treatments and lifestyle modifications. This nuanced understanding of diphenhydramine use acknowledges its potential benefits for immediate symptom relief while emphasizing the importance of avoiding prolonged exposure to its adverse cognitive effects. For individuals who experience occasional allergies or sleep disturbances, diphenhydramine can provide temporary relief. However, for those who rely on it regularly, the risks associated with long-term use outweigh the benefits. Alternative treatments, such as second-generation antihistamines for allergies and cognitive behavioral therapy for insomnia, offer safer and more sustainable solutions. Lifestyle modifications, such as maintaining a regular sleep schedule and creating a conducive sleep environment, can also play a significant role in managing sleep and allergy symptoms without the need for medication. This balanced approach encourages individuals to make informed decisions about their health and to prioritize long-term cognitive well-being over short-term symptom relief.
The increasing awareness of diphenhydramine’s potential risks highlights the need for more research into the long-term effects of over-the-counter medications on brain health. This call for further research underscores the critical gap in our understanding of the cumulative impact of commonly used medications on cognitive function. While some studies have linked diphenhydramine to an increased risk of dementia, more comprehensive research is needed to fully elucidate the underlying mechanisms and to determine the extent of the risk across different populations. Future studies should focus on identifying specific risk factors, such as age, genetics, and pre-existing medical conditions, that may increase an individual’s susceptibility to the adverse cognitive effects of diphenhydramine. Additionally, research is needed to evaluate the effectiveness of alternative treatments and lifestyle modifications in mitigating the need for long-term diphenhydramine use. This concerted research effort will provide valuable insights that can inform clinical practice, public health recommendations, and regulatory policies aimed at protecting and promoting long-term brain health.
FAQ Section:
-
What is diphenhydramine, and what is it used for?
- Diphenhydramine is a first-generation antihistamine widely available over the counter. It works by blocking histamine receptors in the body, reducing allergy symptoms such as sneezing, itching, and runny nose. According to the news source, it is also used as a sleep aid due to its sedative effects. It can be found in products like Benadryl, Unisom SleepGels, and ZzzQuil.
-
What are the potential risks associated with long-term use of diphenhydramine?
- Long-term use of diphenhydramine has been linked to an increased risk of dementia. As Dr. Michael Munger mentioned, the “issue is the cumulative effect” of this medication. Over time, the anticholinergic properties of diphenhydramine can negatively impact cognitive function, leading to memory impairment and an elevated risk of cognitive decline, especially in older adults.
-
Are there safer alternatives to diphenhydramine for treating allergies or insomnia?
- Yes, there are several safer alternatives. For allergy relief, second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are recommended due to their lower anticholinergic effects and reduced risk of cognitive impairment. For insomnia, cognitive behavioral therapy for insomnia (CBT-I) is a non-drug therapy that addresses the underlying causes of sleep problems. Lifestyle adjustments, such as maintaining a regular sleep schedule and creating a conducive sleep environment, can also help.
-
Who is most at risk from the potential cognitive effects of diphenhydramine?
- Older adults are particularly vulnerable to the adverse cognitive effects of diphenhydramine. As people age, their bodies become less efficient at clearing drugs, leading to higher concentrations of diphenhydramine in the system. Older adults also tend to have a reduced supply of acetylcholine, making them more susceptible to the anticholinergic effects of the drug.
-
What should I do if I regularly take diphenhydramine for sleep or allergy relief?
- You should review your medication list, including over-the-counter drugs, and consult with a healthcare provider about any concerns. Discuss safer alternatives and explore potential underlying causes of your sleep or allergy issues. It is essential to have a comprehensive evaluation to minimize reliance on potentially harmful medications and protect your long-term cognitive well-being.
In-Depth Analysis and Expanded Context
The increasing concern over the link between diphenhydramine and dementia is part of a broader awareness of the potential long-term effects of commonly used over-the-counter medications on brain health. For many years, diphenhydramine has been a staple in medicine cabinets, providing quick relief for allergies, cold symptoms, and sleep disturbances. Its accessibility and perceived safety have led to widespread use, often without a full understanding of its potential risks, especially with prolonged consumption.
The implications of the 2015 JAMA Internal Medicine study cannot be overstated. By demonstrating a significant association between cumulative anticholinergic use and an increased risk of dementia, the study prompted a re-evaluation of the risk-benefit profile of medications like diphenhydramine. The anticholinergic effects, which block the action of acetylcholine, a crucial neurotransmitter involved in memory and learning, are now recognized as a significant concern, particularly for older adults whose cholinergic systems are already vulnerable.
The growing body of evidence has led medical professionals and organizations to issue warnings and recommendations aimed at reducing the use of diphenhydramine, especially among older adults. The American Geriatrics Society, for example, includes diphenhydramine on its Beers List, a compilation of medications that are potentially inappropriate for use in older adults due to their high risk of adverse effects. This recommendation reflects the recognition that the risks associated with diphenhydramine use often outweigh the benefits, particularly when safer alternatives are available.
The challenge lies in educating consumers about these potential risks and empowering them to make informed decisions about their health. Many individuals are unaware of the potential long-term cognitive effects of diphenhydramine and may rely on it as a convenient and readily available solution for sleep or allergy symptoms. The lack of prominent warnings on product labels further contributes to this lack of awareness.
To address this issue, healthcare providers play a crucial role in educating patients about the potential risks and benefits of diphenhydramine and in recommending safer alternatives. This includes discussing non-pharmacological approaches, such as cognitive behavioral therapy for insomnia (CBT-I) and lifestyle modifications, as well as alternative medications with lower anticholinergic effects.
For allergy management, second-generation antihistamines like cetirizine, loratadine, and fexofenadine are generally preferred due to their reduced risk of cognitive impairment. These medications selectively target histamine receptors without significantly affecting acetylcholine levels in the brain. However, it’s important to note that even these medications can have some anticholinergic effects, albeit to a lesser extent than diphenhydramine.
CBT-I is a structured program that helps individuals identify and change negative thoughts and behaviors that contribute to insomnia. It typically involves techniques such as stimulus control, sleep restriction, and relaxation training. Studies have shown that CBT-I is highly effective in treating chronic insomnia and can often eliminate the need for medication.
Lifestyle modifications can also play a significant role in improving sleep quality and reducing the need for sleep aids. This includes maintaining a regular sleep schedule, creating a dark, quiet, and cool sleep environment, avoiding caffeine and alcohol before bed, and engaging in regular physical activity during the day.
The broader implications of this issue extend beyond diphenhydramine and highlight the need for greater scrutiny of the potential long-term effects of all over-the-counter medications. Many commonly used OTC drugs have anticholinergic properties, and their cumulative effects on brain health are not fully understood. More research is needed to assess the risks and benefits of these medications and to develop strategies for minimizing potential harm.
Regulatory agencies, such as the FDA, also have a role to play in ensuring that consumers are adequately informed about the potential risks of OTC medications. This includes requiring manufacturers to provide clear and prominent warnings on product labels and to conduct post-market surveillance to monitor the safety of their products.
Ultimately, protecting long-term brain health requires a multi-faceted approach that involves education, research, clinical practice, and regulatory oversight. By raising awareness of the potential risks of diphenhydramine and other anticholinergic medications, promoting safer alternatives, and investing in research, we can help individuals make informed decisions about their health and protect their cognitive well-being.
The current situation underscores the importance of personalized medicine. What might be safe for one person may not be safe for another, depending on their age, medical history, and other medications they are taking. Healthcare providers need to take a holistic approach to patient care, considering all factors that may influence the risk-benefit profile of a particular medication.
The increasing use of electronic health records and data analytics can also play a role in identifying individuals who may be at risk of adverse effects from anticholinergic medications. By analyzing patient data, healthcare providers can identify patterns and trends that may indicate an increased risk of cognitive decline or other adverse outcomes.
In addition to addressing the risks associated with diphenhydramine, it is also important to promote healthy lifestyle habits that can support brain health throughout life. This includes engaging in regular physical activity, maintaining a healthy diet, getting adequate sleep, and staying mentally and socially active.
The focus on diphenhydramine serves as a case study for the broader issue of medication safety and the importance of evidence-based decision-making. By learning from this experience, we can develop better strategies for evaluating the risks and benefits of all medications and for protecting the health and well-being of individuals across the lifespan.
The key takeaway from this news is that while diphenhydramine can provide temporary relief for allergies and sleep disturbances, its long-term use may pose significant risks to cognitive health, particularly in older adults. By exploring safer alternatives, consulting with healthcare providers, and adopting healthy lifestyle habits, individuals can minimize their risk of adverse effects and protect their long-term brain health.
The challenge now lies in translating this knowledge into action. Healthcare providers, regulatory agencies, and consumers all have a role to play in ensuring that medications are used safely and effectively and that the potential risks and benefits are fully understood. By working together, we can create a healthcare system that prioritizes patient safety and promotes long-term health and well-being. The ongoing research and discussions around diphenhydramine highlight the dynamic nature of medical knowledge and the importance of staying informed about the latest findings. As new evidence emerges, it is crucial to adapt clinical practice and public health recommendations accordingly. This iterative process ensures that healthcare decisions are based on the best available information and that patients receive the most appropriate and effective care.