Long-term use of common over-the-counter (OTC) medications containing diphenhydramine, a widely used antihistamine, has been linked to an increased risk of cognitive impairment and dementia, raising concerns among researchers and prompting calls for cautious use, especially among older adults.
A growing body of research suggests that prolonged use of medications with anticholinergic properties, such as diphenhydramine found in popular sleep aids and allergy medications like Benadryl, could negatively impact brain health. Anticholinergics block the action of acetylcholine, a neurotransmitter crucial for memory, learning, and other cognitive functions. While these medications offer relief from allergy symptoms or promote sleep, their impact on cognitive health with long-term use is becoming a significant concern.
The potential link between anticholinergic drugs and cognitive decline has been a subject of scientific scrutiny for years. Studies have shown that individuals who consistently use these medications over extended periods face a higher risk of developing dementia and experiencing cognitive impairment compared to those who do not. The exact mechanism behind this association remains under investigation, but researchers believe that the disruption of acetylcholine signaling in the brain plays a crucial role.
Diphenhydramine is a first-generation antihistamine widely available in various OTC medications used to treat allergies, cold symptoms, and insomnia. While it can effectively alleviate these conditions, its anticholinergic effects are more pronounced than those of newer antihistamines. This means it is more likely to block acetylcholine, potentially leading to cognitive side effects, especially with prolonged use.
The concern is particularly relevant for older adults, who are more susceptible to the adverse effects of anticholinergic drugs. As people age, their bodies become less efficient at clearing medications, leading to higher drug concentrations in the system. Additionally, age-related changes in the brain can make older adults more vulnerable to the cognitive effects of anticholinergics.
According to Dr. Malaz Boustani, a research scientist focused on aging and cognitive impairment at the Regenstrief Institute and Indiana University, the risk is tied to cumulative exposure. “The more you use these drugs, the higher your risk is,” he said. This highlights the importance of considering the duration and dosage of anticholinergic medications when evaluating their potential impact on brain health.
The U.S. Food and Drug Administration (FDA) does not currently have specific warnings about the long-term cognitive effects of OTC diphenhydramine-containing medications. However, healthcare professionals and researchers advocate for increased awareness among consumers and healthcare providers about the potential risks associated with prolonged use. They suggest exploring alternative treatments with fewer anticholinergic effects whenever possible, especially for older adults.
This situation underscores the importance of informed decision-making when using OTC medications. Consumers should carefully read the labels of all medications, understand the potential side effects, and consult with healthcare professionals if they have concerns about long-term use. It is crucial to weigh the benefits of these medications against the potential risks, particularly for individuals who may be more vulnerable to cognitive impairment.
Researchers emphasize that more studies are needed to fully understand the complex relationship between anticholinergic drugs and brain health. However, the existing evidence suggests that cautious use of these medications is warranted, particularly among older adults and individuals with pre-existing cognitive conditions.
For individuals who rely on diphenhydramine-containing medications for sleep or allergy relief, healthcare providers recommend exploring alternative strategies. These may include lifestyle changes, such as improving sleep hygiene or using non-pharmacological allergy treatments. In some cases, newer antihistamines with fewer anticholinergic effects may be a suitable alternative, but it is important to consult with a healthcare professional to determine the most appropriate course of action.
The potential link between diphenhydramine and cognitive decline serves as a reminder that OTC medications are not always risk-free. While they offer convenient and accessible relief from various symptoms, it is essential to use them responsibly and be aware of their potential impact on overall health, especially brain health. The growing body of research on this topic highlights the need for ongoing monitoring and evaluation of the safety of commonly used medications.
Expanded Details and Context:
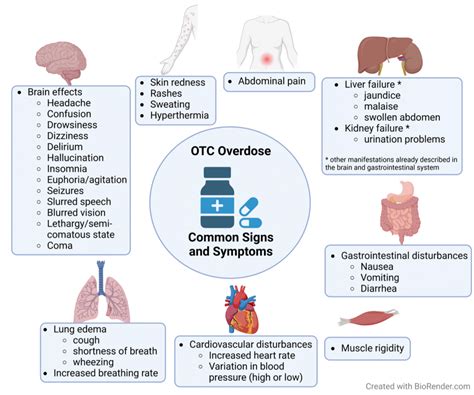
The core concern centers around the anticholinergic properties of diphenhydramine. Anticholinergics work by blocking the action of acetylcholine, a neurotransmitter vital for various bodily functions, including memory, muscle control, and heart rate regulation. While this action can be beneficial in treating certain conditions, such as allergies and motion sickness, it can also lead to undesirable side effects, particularly in the brain.
Acetylcholine plays a critical role in cognitive processes such as memory formation, attention, and learning. By blocking acetylcholine, anticholinergic drugs can impair these cognitive functions, leading to confusion, memory problems, and difficulty concentrating. In the long term, chronic disruption of acetylcholine signaling may contribute to the development of dementia and other cognitive disorders.
Studies have indicated a clear association between the cumulative dose of anticholinergic medications and the risk of cognitive impairment. This means that the longer a person uses these medications and the higher the doses they take, the greater the potential risk to their brain health. This cumulative effect is a key factor in understanding the long-term consequences of anticholinergic drug use.
One significant study published in JAMA Internal Medicine found that individuals who used anticholinergic drugs for three years or more had a significantly higher risk of developing dementia compared to those who did not use these medications. The study also revealed a dose-response relationship, meaning that the risk of dementia increased with higher cumulative doses of anticholinergics.
Another study published in the British Medical Journal analyzed data from over 40,000 individuals and found a similar association between anticholinergic drug use and an increased risk of dementia. The study also identified specific classes of anticholinergic drugs that were particularly strongly linked to cognitive decline, including antihistamines like diphenhydramine.
The elderly are especially vulnerable to the cognitive effects of anticholinergic drugs due to several factors. First, the aging brain undergoes natural changes that can make it more susceptible to the disruptive effects of these medications. Second, older adults are more likely to have age-related medical conditions that may be exacerbated by anticholinergic drugs. Third, older adults often take multiple medications, increasing the risk of drug interactions and adverse effects.
“Older adults are more sensitive to the effects of anticholinergic medications because their bodies process drugs more slowly, and their brains are already more vulnerable to cognitive decline,” explained Dr. Boustani. “It’s crucial for older adults to discuss all of their medications with their healthcare providers, including OTC drugs, to identify potential risks.”
The use of anticholinergic medications can also increase the risk of falls in older adults. These drugs can cause dizziness, drowsiness, and blurred vision, which can impair balance and coordination. Falls are a leading cause of injury and disability in older adults, so it is important to minimize the risk factors, including the use of anticholinergic drugs.
While the risks associated with anticholinergic drugs are well-documented, many individuals are unaware of these potential dangers. OTC medications are often perceived as harmless, and people may not realize that they can have significant side effects, especially with long-term use. This lack of awareness highlights the need for better education and communication about the risks and benefits of all medications, including OTC drugs.
Healthcare providers play a crucial role in educating patients about the potential risks of anticholinergic drugs. They can help patients understand the benefits and risks of these medications, identify alternative treatments with fewer side effects, and monitor patients for signs of cognitive impairment. Pharmacists can also play a valuable role by reviewing patients’ medication lists and identifying potential drug interactions and adverse effects.
“Healthcare providers should routinely review their patients’ medication lists, including OTC drugs, to identify potential anticholinergic risks,” said Dr. Boustani. “They should also educate patients about the potential side effects of these medications and explore alternative treatments whenever possible.”
For individuals who need to take anticholinergic medications, there are several strategies that can help minimize the risks. These include using the lowest effective dose, limiting the duration of use, avoiding other medications with anticholinergic effects, and monitoring for signs of cognitive impairment.
Non-pharmacological approaches can also be effective in managing conditions that are often treated with anticholinergic drugs. For example, lifestyle changes such as improving sleep hygiene, managing stress, and engaging in regular exercise can help improve sleep quality without the need for sleep aids. Similarly, allergy symptoms can often be managed with non-pharmacological treatments such as nasal irrigation, air purifiers, and allergen avoidance.
The FDA plays a critical role in regulating the safety of medications, including OTC drugs. The agency requires manufacturers to include warnings about potential side effects on medication labels. However, some experts argue that the current warnings about the cognitive effects of anticholinergic drugs are not prominent enough and that more needs to be done to educate consumers about these risks.
“The FDA should consider strengthening the warnings about the cognitive effects of anticholinergic drugs on medication labels,” said Dr. Boustani. “They should also work with healthcare providers and consumer organizations to raise awareness about these risks.”
Researchers continue to investigate the complex relationship between anticholinergic drugs and brain health. Future studies will focus on identifying specific mechanisms by which these drugs affect cognitive function, determining which individuals are most vulnerable to their effects, and developing strategies to prevent or mitigate the cognitive risks associated with their use.
The information currently available underscores the importance of making informed decisions about medication use, particularly for older adults and those with pre-existing cognitive conditions. Consulting with healthcare professionals, carefully reading medication labels, and exploring alternative treatments are essential steps in protecting brain health.
The growing body of research on the potential risks associated with long-term use of common OTC drugs containing diphenhydramine serves as a wake-up call. It highlights the need for greater awareness, more cautious prescribing practices, and ongoing research to fully understand the impact of these medications on cognitive health. By taking these steps, we can help ensure that individuals can safely manage their health conditions without compromising their brain health.
The potential link between common OTC medications like Benadryl and cognitive decline is not just a medical issue; it’s a public health concern. Millions of people rely on these medications for relief from allergies, insomnia, and other common ailments. Understanding the potential risks associated with their long-term use is crucial for making informed decisions and protecting brain health.
Frequently Asked Questions (FAQs):
1. What is diphenhydramine, and what is it used for?
Diphenhydramine is a first-generation antihistamine commonly found in over-the-counter (OTC) medications. It is used to treat a variety of conditions, including:
- Allergies: Relieves symptoms such as runny nose, sneezing, itchy eyes, and hives.
- Cold and flu symptoms: Helps to dry up nasal passages and reduce coughing.
- Insomnia: Acts as a sleep aid by causing drowsiness.
- Motion sickness: Prevents nausea and vomiting associated with travel.
- Itching: Relieves itching caused by insect bites, poison ivy, and other skin irritations.
2. How does diphenhydramine affect the brain?
Diphenhydramine is an anticholinergic drug, which means it blocks the action of acetylcholine, a neurotransmitter crucial for memory, learning, and other cognitive functions. By blocking acetylcholine, diphenhydramine can impair cognitive processes, leading to:
- Confusion: Difficulty thinking clearly and making decisions.
- Memory problems: Trouble remembering recent events or learning new information.
- Difficulty concentrating: Inability to focus attention on tasks.
- Drowsiness: Feeling sleepy and sluggish.
Long-term use of diphenhydramine may contribute to the development of dementia and other cognitive disorders.
3. What are the risks associated with long-term use of diphenhydramine?
Long-term use of diphenhydramine has been linked to an increased risk of:
- Cognitive impairment: Decline in cognitive functions such as memory, attention, and executive function.
- Dementia: A progressive decline in cognitive abilities that interferes with daily life.
- Falls: Increased risk of falls due to dizziness, drowsiness, and blurred vision.
- Other side effects: Dry mouth, constipation, blurred vision, and urinary retention.
The risks associated with long-term use of diphenhydramine are greater for older adults and individuals with pre-existing cognitive conditions.
4. What are some alternatives to diphenhydramine?
There are several alternatives to diphenhydramine, depending on the condition being treated:
- For allergies: Newer, non-sedating antihistamines such as cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) have fewer anticholinergic effects and are less likely to cause cognitive impairment. Nasal corticosteroids and other allergy medications may also be effective.
- For insomnia: Lifestyle changes such as improving sleep hygiene, managing stress, and engaging in regular exercise can help improve sleep quality without the need for sleep aids. Melatonin supplements and cognitive behavioral therapy for insomnia (CBT-I) may also be helpful.
- For motion sickness: Non-drowsy antihistamines such as meclizine (Bonine) and dimenhydrinate (Dramamine) can prevent nausea and vomiting associated with travel. Ginger and acupressure wristbands are also effective non-pharmacological treatments.
- For itching: Topical corticosteroids and antihistamine creams can relieve itching caused by insect bites, poison ivy, and other skin irritations. Calamine lotion and oatmeal baths may also be helpful.
It is important to consult with a healthcare professional to determine the most appropriate treatment for your specific condition.
5. What should I do if I am currently taking diphenhydramine regularly?
If you are currently taking diphenhydramine regularly, it is important to:
- Talk to your healthcare provider: Discuss the potential risks and benefits of continuing to take diphenhydramine. Your healthcare provider can help you determine if there are safer alternatives available.
- Review your medication list: Make sure your healthcare provider is aware of all the medications you are taking, including OTC drugs and supplements. This will help identify potential drug interactions and adverse effects.
- Use the lowest effective dose: If you need to continue taking diphenhydramine, use the lowest dose that provides relief from your symptoms.
- Limit the duration of use: Avoid taking diphenhydramine for extended periods of time. If your symptoms persist, consult with your healthcare provider.
- Monitor for signs of cognitive impairment: Pay attention to any changes in your memory, attention, or cognitive function. If you experience any of these symptoms, contact your healthcare provider.
- Consider non-pharmacological alternatives: Explore lifestyle changes and other non-pharmacological treatments to manage your symptoms.
- Do not stop taking any medication without consulting your doctor.
By taking these steps, you can help minimize the risks associated with diphenhydramine and protect your brain health.